3885 S. Decatur Blvd Suite #1080
Las Vegas, NV 89103


Managing gout attacks involves a combination of lifestyle changes and medical treatments to reduce uric acid levels and prevent flare-ups. Gout, once known as a disease of kings due to its association with rich foods and alcohol, is now widespread, affecting over eight million US adults. The rise in cases is also linked to obesity and high blood pressure. Gout is caused by uric acid crystals in the joints, leading to intense pain, redness and swelling, commonly in the big toe. Prevention strategies include losing weight, avoiding alcohol and high-purine foods like red meat and seafood, and incorporating low-fat dairy into your diet. Medications to lower uric acid levels are often necessary and regular use of them can significantly reduce the frequency and severity of gout attacks. These measures can improve the quality of life and prevent long-term joint damage. If you have symptoms of gout, it is suggested that you schedule an appointment with a podiatrist for help in managing it effectively.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Loren Hansen, DPM from Ankle & Foot Medical Center. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Gout is a form of arthritis that is caused by a buildup of uric acid crystals in the joints. This considered to be one of the most frequently recorded medical illnesses throughout history. Gout occurrences in the US have risen within the past twenty years and the condition now affects 8.3 million people which is 4% of all Americans. Researchers have found that gout affects men more than women and African-American men more than white men.
Symptoms of gout are warmth, swelling, discoloration, and tenderness in the affected joint area. The small joint on the big toe is the most common place for a gout attack to occur.
People who are obese, gain weight excessively, drink alcohol heavily, have high blood pressure, or have abnormal kidney function are more likely to develop gout. Furthermore, certain drugs and diseases are likely to increase levels of uric acid in the joints which eventually leads to gout. You are also more likely to develop gout if you eat a lot of meat and fish.
Many who experience gout attacks will experience repeated attacks over the years. Some people who have gout symptoms, may never have them again, but others may experience them several times a year. If you have gout symptoms throughout the year, you may have recurrent gout. Those who have gout should also be careful about their urate crystals collecting in their urinary tract, because this may lead to kidney stones.
Diagnosis for gout is done by checking the level of uric acid in the joints and blood. Your podiatrist may also prescribe medicine to reduce uric acid buildup in the blood, which will help prevent any gout attacks.
To treat gout, your podiatrist may also prescribe you Anti-inflammatory medication (NSAIDs) which will relieve the pain and swelling of a gout episode and it can also shorten a gout attack. Maintaining a healthy diet is also a proven method to prevent gout attacks.

Flat feet occur when the arch of the foot collapses, causing the entire foot to make contact with the ground. This condition can arise from genetics, trauma, or underlying health issues like diabetes. While many people with flat feet manage symptoms through nonsurgical treatments, surgery may become necessary when these interventions fail to provide relief. Complications from flatfoot can include changing the way you walk, plantar fasciitis, and Achilles tendonitis, which can significantly impact daily activities. Custom orthotics, bracing, stretching exercises, and certain medications can help to alleviate pain and improve foot function. But when these measures are insufficient, a podiatrist may recommend surgical reconstruction to restore the foot's arch and alleviate discomfort. Surgery typically involves repairing or reconstructing tendons and ligaments, realigning bones, or fusing joints to create a stable arch. Because recovery from flatfoot surgery can take up to three months, carefully following post-operative care instructions is paramount to a successful outcome. If you have severe pain from flat feet, it is suggested that you schedule an appointment with a podiatrist who can determne if surgery is right for you.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Loren Hansen, DPM from Ankle & Foot Medical Center. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flatfoot is a foot disorder that is not as straightforward as many people believe. Various types of flatfoot exist, each with their own varying deformities and symptoms. The partial or total collapse of the arch, however, is a characteristic common to all types of flatfoot. Other signs of flatfoot include:
One of the most common types of flatfoot is flexible flatfoot. This variation usually starts in childhood and progresses as one ages into adulthood. Flexible flatfoot presents as a foot that is flat when standing, or weight-bearing. When not standing, the arch returns. Symptoms of flexible flatfoot include:
Your podiatrist will most likely diagnose flatfoot by examining your feet when you stand and sit. X-rays may be taken to define the severity and help determine the treatment option best for your condition. Nonsurgical treatments can include activity modification, weight loss, orthotics, immobilization, medications, physical therapy, shoe modifications, and ankle foot orthoses (AFO) devices. If nonsurgical methods prove ineffective, surgery may be considered. Multiple surgical procedures can correct flatfoot; and depending on your specific condition, one may be selected alone or combined with other techniques to ensure optimal results.
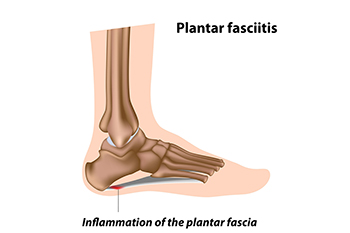
The plantar fascia is a thick band of tissue that connects the heel to the toes. Plantar fasciitis, an inflammation of this tissue, can stem from various biomechanical factors. Problems like an abnormal lower leg structure, limited ankle movement, and inward or outward heel or foot angles can strain the plantar fascia. These abnormalities can alter foot mechanics, leading to excessive tension and micro-tears in the fascia. Symptoms include sharp heel pain, especially after prolonged periods of standing or walking, which tends to improve with rest but worsens upon resuming activity. Early morning stiffness and tenderness in the heel or arch are also common. Addressing these biomechanical issues through proper footwear, orthotics, stretching exercises, and avoiding excessive strain on the feet can help to manage symptoms and prevent recurrence of this ailment. If you have been afflicted by plantar fasciitis, it is suggested that you confer with a podiatrist who can offer you various effective treatment methods.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Loren Hansen, DPM from Ankle & Foot Medical Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
 A hairline fracture, or stress fracture, is a small crack or severe bruise within a bone that is common among athletes that are involved in running and jumping. People with osteoporosis are also more prone to developing hairline fractures. These injuries typically result from overuse or repetitive stress, often worsened by inadequate healing time between activities. The bones in the foot are particularly susceptible to stress fractures due to their role in absorbing impact during physical activities. Within the foot, the second and third metatarsals are frequently affected, as well as the heel, ankle bones, and navicular bone. Symptoms primarily include pain that worsens with activity and subsides with rest, swelling, tenderness, and bruising. Factors that can increase the risk of developing a stress fracture include participation in high-impact sports, certain foot structures, and weakened bones due to conditions like osteoporosis. Previous fractures, nutritional deficiencies, and improper equipment or techniques are other risk factors. Diagnosing a stress fracture often involves a physical exam and may require imaging tests like MRIs or bone scans, as X-rays might not detect fractures. If ignored, a stress fracture can worsen into a complete break. If you are experiencing foot pain during exercise, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
A hairline fracture, or stress fracture, is a small crack or severe bruise within a bone that is common among athletes that are involved in running and jumping. People with osteoporosis are also more prone to developing hairline fractures. These injuries typically result from overuse or repetitive stress, often worsened by inadequate healing time between activities. The bones in the foot are particularly susceptible to stress fractures due to their role in absorbing impact during physical activities. Within the foot, the second and third metatarsals are frequently affected, as well as the heel, ankle bones, and navicular bone. Symptoms primarily include pain that worsens with activity and subsides with rest, swelling, tenderness, and bruising. Factors that can increase the risk of developing a stress fracture include participation in high-impact sports, certain foot structures, and weakened bones due to conditions like osteoporosis. Previous fractures, nutritional deficiencies, and improper equipment or techniques are other risk factors. Diagnosing a stress fracture often involves a physical exam and may require imaging tests like MRIs or bone scans, as X-rays might not detect fractures. If ignored, a stress fracture can worsen into a complete break. If you are experiencing foot pain during exercise, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Loren Hansen, DPM from Ankle & Foot Medical Center. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.

Cracked heels are caused by various lifestyle factors and medical reasons. Prolonged standing, wearing open-backed shoes, and walking barefoot on hard surfaces can contribute to the development of dry, cracked skin on the heels. Medical conditions such as diabetes, thyroid disorders, and eczema can also lead to cracked heels by causing dryness and reducing the skin's natural elasticity. To help prevent cracked heels, apply a thick, hydrating lotion to keep the feet moisturized. Wearing supportive, closed-back shoes can help reduce pressure on the heels. Additionally, using a pumice stone to gently exfoliate dead skin and avoiding walking barefoot on hard surfaces can be beneficial. If you have developed cracked heels, it is suggested that you consult a podiatrist who can effectively treat this condition, which may include prescribed medicine.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Loren Hansen, DPM from Ankle & Foot Medical Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
Ways to Prevent Cracked Heels
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Las Vegas, NV . We offer the newest diagnostic and treatment technologies for all your foot care needs.